High-end retailers now flaunt their exorbitant price markups for products without experiencing dips in sales so why doesn’t our healthcare system?
According to the New York Times‘ article, ‘Revealing Costs to Make Sales’ the leather goods company, Oliver Cabell posts the cost breakdown of all its products on its website so customers can see exactly what they are playing for and how much the manufacturer is charging them on top of its cost of production.
For the record, Oliver Cabell spends $16.02 on canvas, $11.58 on leather, $5.68 on lining and 78 cents on webbing and $4.27 for the zipper.
This practice, known as transparent pricing, has been gaining hold among a select group of retailers, who say that it appeals in particular to millennials – who often want to know exactly what they’re paying for. Guess what? So do the rest of us!

I’m confident that most ‘divabetics’ would also like to know why the fashion industry’s transparent pricing isn’t available in our healthcare system especially since the costs of meds (like insulin), doctor’s visits and/or equipment keep rising.
Seriously, wouldn’t it be great to see the price tag for a treatment ahead of time and determine how much you’re willing to pay out-of-pocket before receiving care?
“Pricing transparency and stories behind the scenes help the shopper navigate the decision to pay for a more expensive product,” said Natalie Grillon, founder of Project Just, which collects ethics and sustainability date on fashion brands.
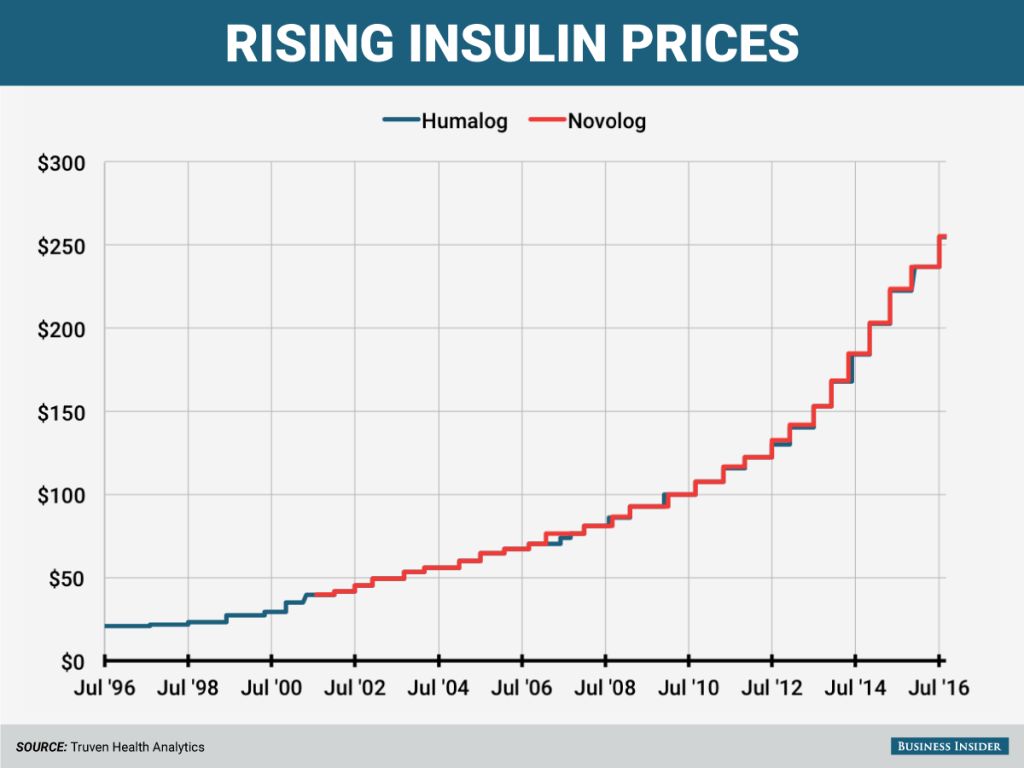
Find out What’s Behind the Rising Price Tag for Insulin
I’m sure I’m not the only one who would like to know what’s behind the rising prices of insulin prices — increases that mean some people are spending as much on monthly diabetes-related expenses as their mortgage payment.
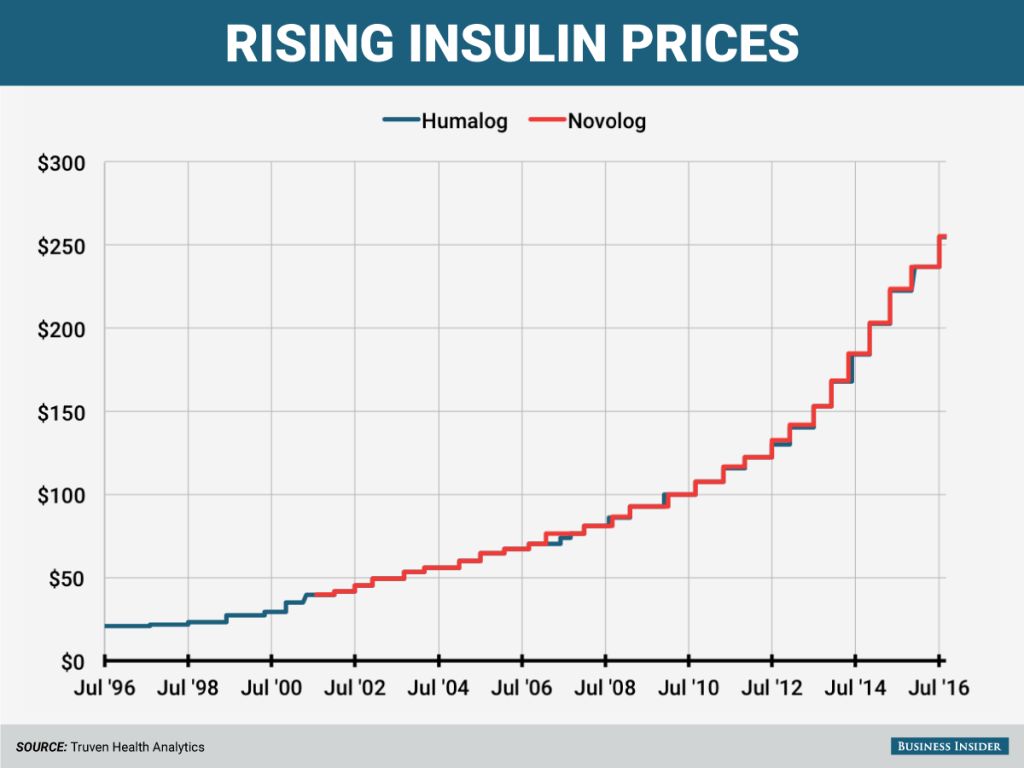
As of May 2, the list price of Humalog, a short-acting insulin, is $274.70 for a 10 ml bottle, an increase of 7.8% from what the list price had been since July 2016. On May 2, Lilly also took a 7.8% list price increase to Humulin, an older form of insulin. Novo Nordisk, which also makes a short-acting insulin, increased its prices to the drug in 2017. In February, the drugmaker raised its price to $275.58 for a 10 ml bottle, up 7.9% from what the list price had been since July 2016. In December, Novo Nordisk committed to limiting all future drug list price increases from the company to single digit percentages.
Over the last decade, the list prices of the two drugs have increased by 290%. READ MORE
Apparently most Americans want greater price transparency and would compare health care prices if given the option according to Public Agenda.
The historical opacity of health care prices is widely believed to be a major factor inhibiting the more efficient functioning of the delivery system,” according to the Robert Wood Johnson Foundation. “Health economists and other experts are convinced that significant cost containment cannot occur without widespread and sustained transparency in provider prices.”
Unfortunately, ore than half of Americans say they have tried unsuccessfully to find out about the price of health care before getting care according to Public Agenda.
The vast majority of people believe that more expensive care does not equate to better care. This demonstrates the demand for transparency among consumers, and the recognition among consumers that price variation in health care is often an arbitrary divide that does not necessarily reflect quality of care.
With health premiums increasing, families have to make more educated purchasing decisions in the health marketplace to save money, especially those families with higher deductibles. But accurate price information is hard to come by considering the default price opacity in most states. The Healthcare Financial Management Association cites a recent report where the U.S. Government Accountability Office asked dozens of health care providers about their price for a knee replacement. The estimates given ranged from $33,000 to $101,000. This wide range in prices is difficult to account for, and without more comprehensive price transparency, consumers face a difficult time choosing the most cost-efficient option.
One way you can help your state government combat price opacity is by contacting your elected officials to request providers and insurance personnel to talk about pricing, as well as guiding people toward reliable price information and explaining to them how prices vary across providers. READ MORE

How to Make the Most of Your Next Doctor’s Visit
If you really want to take full advantage of your doctor visit, plan in advance. Here are two key points from One Drop will make for a very informed doctor’s visit:
Check out your blood glucose (BG) stats from for the past month before heading to the doctor. What’s your average BG level? % high, % low? How does your food intake affect these numbers? Do you have lots of high BGs (“hypers”) or lows BGs (“hypos”)? If so, are they occurring often? Are you finding trends or patterns? How severe are they? Can you feel the early signs of a low and take action before it becomes too severe? What do you eat/drink to treat them? How quickly does your body respond? When do you get the most severe highs (highest glucose levels)? Is that associated with food, medications, activity, all three, or other factors (stress, illness)? Any idea what may be causing these highs and lows?
(Pro Tip  : if you’re taking insulin, One Drop provides the average total daily insulin and the breakdown into %basal and %bolus insulin.) What’s your average daily activity, and how does that seem to be affecting BG numbers?
: if you’re taking insulin, One Drop provides the average total daily insulin and the breakdown into %basal and %bolus insulin.) What’s your average daily activity, and how does that seem to be affecting BG numbers?
Discuss your mood! A topic often overlooked at doctor’s appointments, mental health is something that should take tip-top-priority on your talking points list. How are you doing psychologically? How does diabetes affect you mentally? Are your major highs/lows taking a toll on you psychologically?
Remember, this is your time. Don’t be bashful with your questions. Come prepared, and you’ll be able to make any and all necessary changes. READ MORE
TUNE IN: Tuesday, June 13, 2017 for Diabetes Late Nite with music by Maxwell. We’re talking about Diabetic Macular Edema (DME) with musical inspiration from Maxwell. Guests include singer Alfa Anderson, Diabetic Macular Edema patient Maryanne Kass, Artist Bryce Chisholm, the Charlie’s Angels of Outreach, Poet Lorraine Brooks and Mama Rose Marie. Throughout the podcast we will be featuring selected songs from several of several of Maxwell’s albums courtesy of SONY Music.











 : if you’re taking insulin, One Drop provides the average total daily insulin and the breakdown into %basal and %bolus insulin.) What’s your average daily activity, and how does that seem to be affecting BG numbers?
: if you’re taking insulin, One Drop provides the average total daily insulin and the breakdown into %basal and %bolus insulin.) What’s your average daily activity, and how does that seem to be affecting BG numbers?