If you love knowing that a book is based on real life before you dive in, you’re in luck! I just finished the first draft of my next ‘Mister Divabetic Mystery: One Murder Tutu Many’, based on my own dietary restrictions.
I’ve been gluten free under the watchful eye of my doctor for two weeks. She thinks my new diet will help alleviate some of the discomfort I experience from psoriasis. During the winter months in New York City my psoriasis especially flares up so I decided it was worth a try!
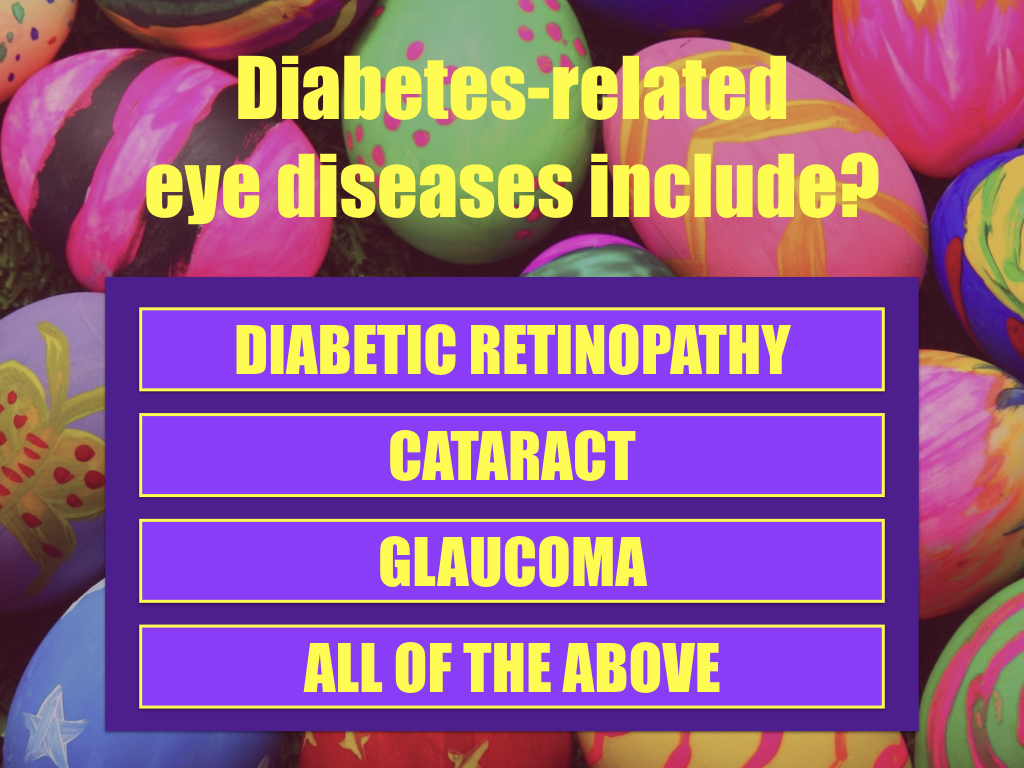
Gluten is a protein found in wheat, rye, barley, and other related grains. It’s also found hiding in shocking amount of other foods including ketchup, soy sauce, coffee creamer! Those who are genuinely intolerant have an autoimmune condition known as celiac disease, where their immune system responds to the gluten protein by attacking the small intestine. The link between celiac disease and type 1 diabetes mellitus is well known.
Common symptoms of malabsorption include gas, bloating, diarrhea, and weight loss. Other symptoms may include fatigue, anemia, irritability, or depression. In many cases of undiagnosed celiac disease, however, there are no symptoms at all.
Once diagnosed, the only treatment of celiac disease is lifelong, complete elimination of gluten-containing foods from the diet. With gluten elimination, symptoms may disappear within a few days, but complete healing of the small intestine may take three to six months or, in some cases, up to two years.
The good news for me, someone who doesn’t have celiac, is that I’m seeing a slight difference in my psoriasis. It hasn’t disappeared but it has stopped itching and some patches (on my shoulders and elbows) are now slightly smaller in size.
The bad news is a recent Harvard University study found that people who limited their gluten intake or avoided it completely actually had a 13 percent higher chance of developing type 2 diabetes. I have a family history of diabetes so this news immediately caught my eye!
“We wanted to determine if gluten consumption will affect health in people with no apparent medical reasons to avoid gluten,” explained Dr Geng Zong of Harvard’s School of Public Health. “Gluten-free foods often have less dietary fiber and other micronutrients, making them less nutritious and they also tend to cost more.”
Fiber is known to protect against type 2 diabetes. When the researchers had adjusted for the protective effect of fiber, they found those in the top 20 percent for consuming gluten in their study had a 13 percent less chance of developing type 2 diabetes, compared to those who consumed 4 grams or less.
After reading the report I’ve become conscious of adding more fiber to my diet. It’s that hard to do even if you’re gluten free! I’m eating more vegetables (the crunchier the better), nuts, berries, beans and brown rice.
Occasionally when I crave something sweet I now make myself a treat. Here’s a great mini cheesecake recipe I found online at my baking addiction. The author, ‘Erin’ claims, ”these fuss-free gluten-free mini cheesecakes are perfect for parties or potlucks and couldn’t be any easier to make!” After making them, I agree! Click the link for the recipe: Gluten-Free Mini Cheesecakes Recipe from ‘My Baking Addiction’
By the way, I liked this recipe so much it plays a significant role into next year’s Mister Divabetic Mystery: ‘One Murder Tutu Many’ podcast/short story set in the world of ballet.
Can’t wait until next year to hear one of my ‘Mister. Divabetic Mysteries podcasts? Click on the link to enjoy ‘Phantom of the Okra’ featuring music from ‘Phantom of the Opera’ courtesy of SONY Music. A trip to the local Farmer’s Market turns into a fiasco for the happy healthcare host when he finds a dead body in a bushel of okra in the Mr Divabetic Mystery podcast,’Phantom of the Okra’ LISTEN