We’re talking about coping with diabetes, depression and shame during the holidays on Divabetic’s podcast with musical inspiration from Leona Lewis.
‘Tis the season for family, festivity, and temptations that may disrupt daily diabetes health routines. That means it’s also the season when eating healthy, staying active, and taking medication on schedule is more challenging. The added stress and anxiety of staying on track with your diabetes self-care may cause even those who are usually content to experience loneliness, anxiety, and a lack of fulfillment.
Several studies show that people with diabetes have a greater risk of depression than people without diabetes.
Just like denial, depression hinders good intentions in self-care. It can even make it harder to do things you enjoy.
“I have a best friend who has severe depression, who takes medication and still struggles, so I know how bad it can be,” says Leona Lewis.
Leona’s friend describes herself as having “highs and lows” brought on by circumstance, not a clinical illness.
If you’re feeling down, remember you’re not alone. It’s important to share your feelings with your healthcare team. Seeking help takes courage and can be the first step toward feeling better.
Leona Lewis’ holiday song, One More Sleep, sparks our discussion about how the holidays affect your sleep. Insomnia during the holidays is quite common. The holidays bring parties, overeating, later bedtimes, shopping, overspending, and traveling, which may bring on jet lag. The financial pressures associated with gift-giving can also cause sleep disruption during the holidays.

Changing your behaviors and attitudes and adding more physical activities can go a long way toward eliminating insomnia so you can enjoy a deserved and joyous holiday season.
Traveling or spending time with family can shake up our usual meal routines, too. Megrette Fletcher, a diabetes educator, mentioned in an interview that everything changes and can be quite stimulating when we’re away from home, which might lead us to let our guard down a bit. Common sense says eating too much doesn’t improve the food experience, but when faced with an array of delicious treats, it can be hard to resist. As Megrette says, “Food is part of the enjoyment.” Just because you can’t take the food home with you doesn’t mean you have to eat everything in sight if you’re already full. It’s okay to savor the moment and stop when you’ve had enough!
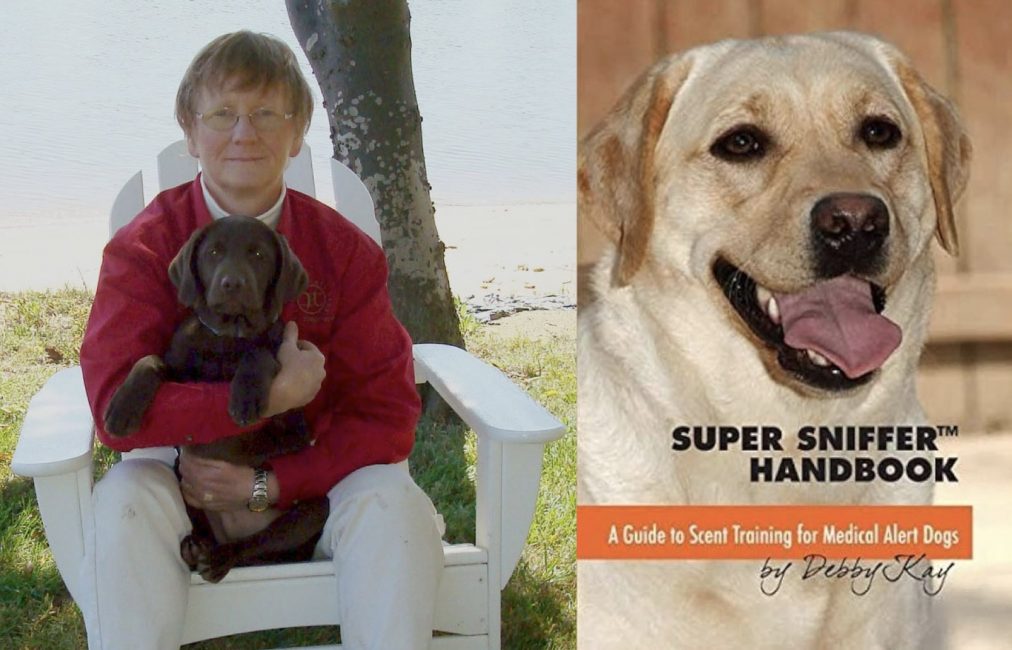
We also have some fantastic guests on the Divabetic podcast, including experts like Debby Kay and Megrette Fletcher, and inspiring people like singer Leona Lewis, who will be sharing her music from the Christmas, with Love album. Plus, don’t miss our chance to win 6 months of mySugr Pro access in our INSTANT WINNER challenge!
Throughout the podcast, we will feature music from Leona Lewis’s Christmas, with Love album courtesy of SONY Music.